Health authorities have confirmed that a case of a rare strain of mpox has been detected in Southern Queensland.
The patient is being treated at Logan Hospital and there is no particular concerns for their health. They acquired the virus in central Africa, and authorities say its unlikely there will be any secondary transmission.
Queensland Health says the patient has the clade 1 mpox strain, which is known to cause more severe illness.
“The community can be assured that exposure to members of the community has been very limited and the public should not be concerned,” it said.
“Mpox does not spread easily between people and is mainly spread through very close or intimate contact with someone infected.” the Health Department said in its advice, as they announced contact tracing was underway.

Health Minister Tim Nicholls said close to 60 people the man had been in contact with had already been identified.
“He was not contagious on the return journey to Australia from Africa and those close contacts that he has been in contact with, including at the emergency ward and in other locations, are being contact traced right now and identified,” Nicholls said.
The Minister said the department had identified 19 community contacts, including members of the man’s family, and 40 hospital staff contacts.
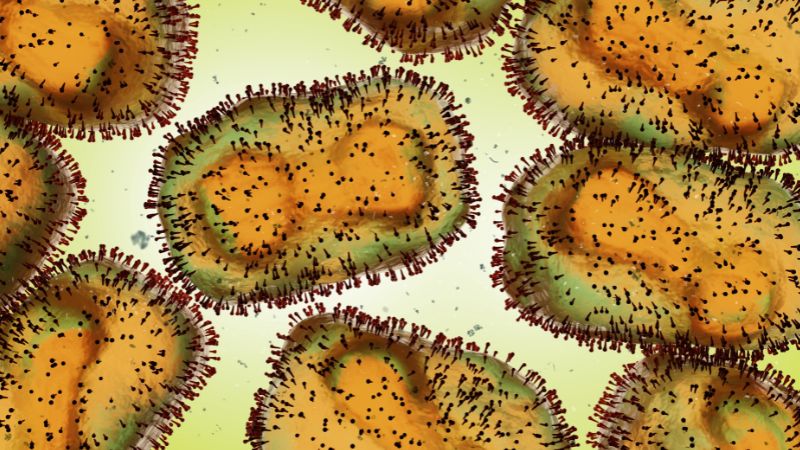
Mpox is an infection caused by the monkeypox virus, a virus that belongs to the same family as the smallpox virus but generally causes a milder illness.
There are two ‘clades’ of the virus – clade I and clade II. Clade II is generally associated with milder illness and was responsible for the 2022 global outbreak.
The World Health Organization declared a Public Health Emergency of International Concern on 14 August 2024 for an outbreak of mpox clade I cases in Central and West Africa. So far two cases of clade I mpox have been detected in Australia.
Most people who have mpox experience a mild illness and fully recover within 2-4 weeks. Symptoms start within three to 21 days of exposure to the virus and may include a rash, pimples, or sores, which later develop into fluid-filled lesions, pustules, or ulcers. Some people also have fever, headache, muscle aches, backache, or enlarged lymph glands.
People who have any symptoms of mpox should avoid close or intimate contact, including sex, with other people and see their doctor. They should ask their doctor if it could be mpox, so they can be tested.
Mpox is most commonly spread through sexual or intimate contact but can also be spread through any skin-to-skin contact, contact with contaminated items such as bedding and towels, and rarely, through breathing in droplets from coughs and sneezes.
The mpox vaccine is free for those at higher risk including sexually active men who have sex with men and their sexual partners, as well as sex workers and their sexual partners.
Two doses at least a month apart are required for optimal protection.
People can help prevent the spread of mpox by avoiding sex if they have any signs of sores or blisters, limiting sexual partners, and keeping contact details of new partners to help with contact tracing if needed. Condoms offer some protection, but only protect the area of skin covered.
For more information and support, including options for testing, go to Monkeypox (healthywa.wa.gov.au) or Mpox resources – communications toolkit (health.wa.gov.au).
Contact the sexual health hotline on 9227 6178 (metro) or 1800 198 205 (country).